Clinically, VVA is manifested by dryness in the vagina, dyspareunia, vaginal discharge, itching, and pain.
Dyspareunia leads to a decrease in sex drive and fear of sexual intercourse. As the frequency of coitus diminishes, vaginal lubrication declines further. Some women may already have narrowing of the vagina or manifestations of vaginismus, limiting penetration into the vagina. However, in some women with mild-to-moderate severity, VVA occurs asymptomatically, and verification of diagnosis is possible only with vaginal examination.
The diagnosis of VVA1 is made difficult by the low awareness of women about the pathological manifestations of the postmenopausal period and unwillingness/embarrassment to discuss the symptoms of an intimate character with the expert. In their study, Nappi and Kokot-Kierepa noted that only 4% of respondents associated their symptoms with the manifestations of menopause. Unfortunately, 75% of patients with the clinical manifestations of VVA do not seek help from specialists.2
The experts in the field of women’s health are faced with the task of early detection of VVA and the timely administration of treatment.
A detailed history of the patient with a suspicion of VVA should be conducted to identify other possible causes, including effects of irritants (lubricants, hygienic gels, soaps, spermicides), the use of antiestrogen drugs, advanced oophorectomy, or chemotherapy.
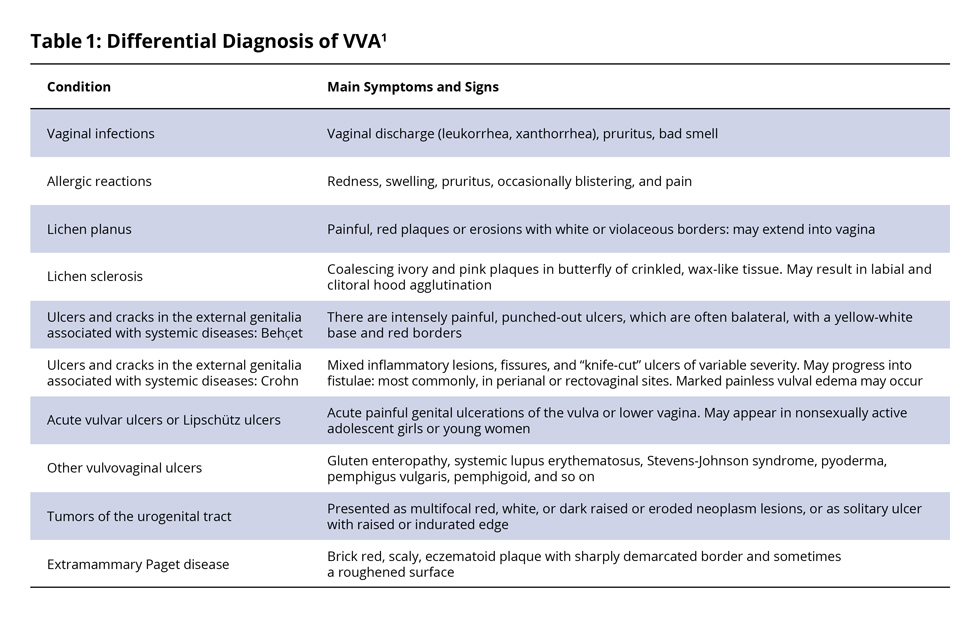
A differential diagnosis should consider the conditions summarised in Table 1.
References
1. Naumova, I. and Castelo-Branco, C. 2018 ‘Current treatment options for postmenopausal vaginal atrophy’, International Journal of Women’s Health. Volume 10, 387-395.
2. Nappi, R.E. and Kokot-Kierepa, M. Vaginal Health: Insights, Views & Attitudes (VIVA)—Results from an International Survey. Climacteric. 2012; 15: 36-44.