Vulvar and vaginal atrophy (VVA) is a relatively common condition symptomatically affecting approximately 50% of all postmenopausal women.1
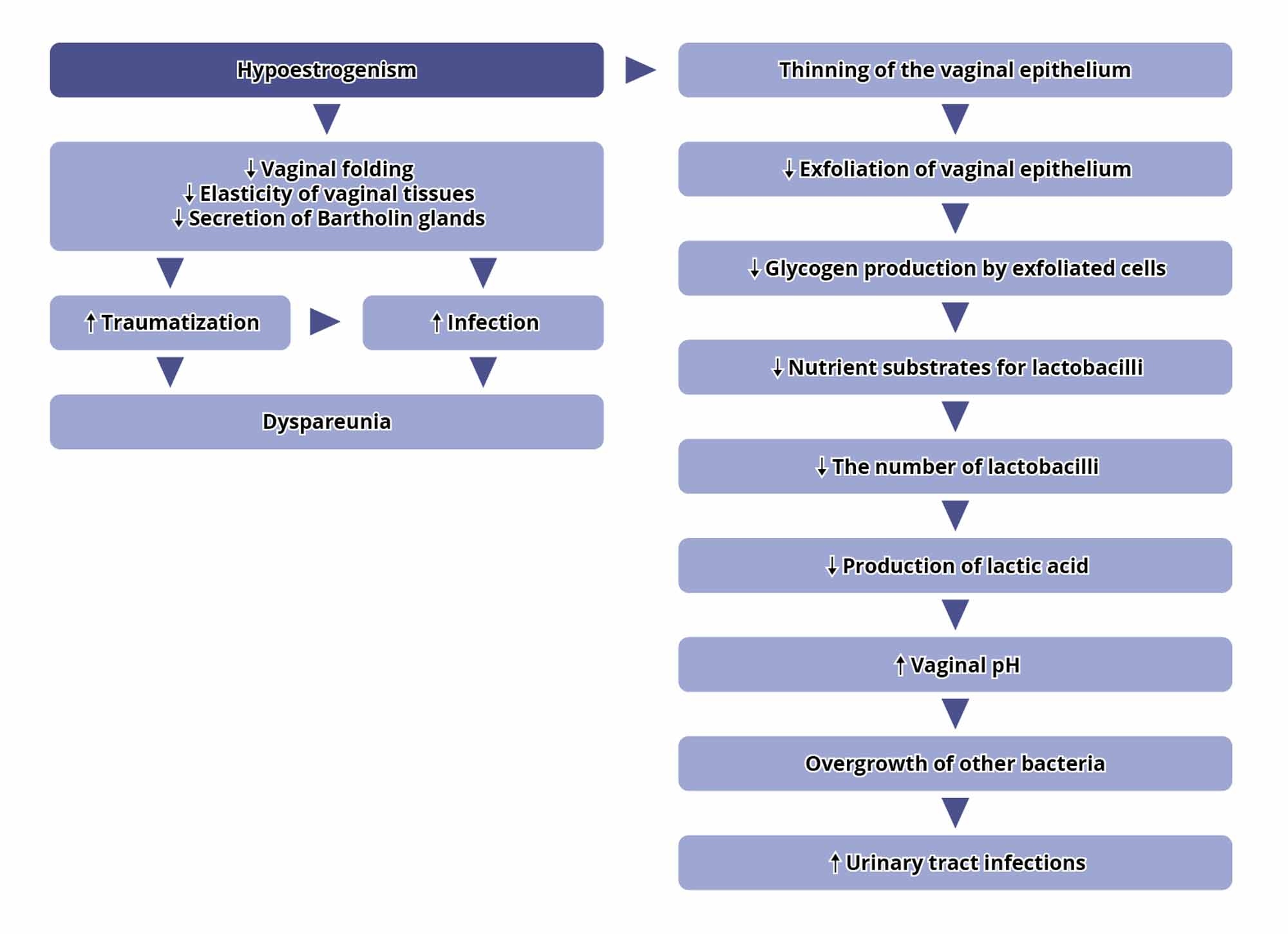
Under hypoestrogenic conditions, the vaginal epithelium becomes thinner, its barrier function is lost, the vaginal folding decreases, the elasticity of the tissues decreases, and the secretory activity of the Bartholin glands decreases, which lead to traumatisation of the vaginal mucosa and painful sensations – see Figure 1.2 These changes in vaginal epithelium also cause changes in the vaginal microbiota, resulting in increased urinary tract infections.
Figure 1. Cascade Effects of the Mechanism of VVA2
Symptoms of VVA
Symptoms of vaginal estrogen deficiency most commonly include vaginal dryness (75%), dyspareunia (40%), vulval and vaginal pruritis and discharge.
The urinary tract is also commonly affected, leading to urinary frequency and urgency, nocturia, dysuria and incontinence. Recurrent urinary tract infections occur in up to 20% of postmenopausal women because of atrophy of the urothelium in response to estrogen deficiency.3
VVA Clinical findings
Clinical findings include atrophy of the labia majora and vaginal introitus.
The labia minora may recede. Vulvar and vaginal mucosae may appear pale, shiny, and dry; if there is inflammation, they may appear reddened or pale with petechiae. Vaginal rugae disappear, and the cervix may become flush with the vaginal wall. Vaginal shortening and narrowing tend to occur.4
The Vaginal Health Index is commonly used by clinicians to rate both the appearance of the vaginal mucosa and production of secretions on a scale of 1–5. In 2014, the North American Menopause Society/International Society for the Study of Women’s Sexual Health Consensus Panel introduced the Genitourinary Syndrome of Menopause (GSM), an overarching terminology that describes various menopausal symptoms and signs including genital, sexual and urinary symptoms.
The GSM assessment tool considers three categories of elasticity, lubrication, and tissue integrity; an anatomical section that includes vulval, vaginal and urethral anatomy; and two objective measures, vaginal pH, and vaginal maturation.
These seven components each receive a score from 0–3 based on severity of the condition. A total score is then calculated by adding each of the scores together to give a total out of 21. A score of 0–7 is considered to be mild atrophy, 7–14 moderate atrophy and >14 severe atrophy. The score system refers to the degree of atrophy rather than the ‘syndrome’ itself.3
References
1. Nappi, R.E. et. al. 2016 ‘Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE Survey’, Climacteric. Volume 19, No.2, 188-197
2. Naumova, I. and Castelo-Branco, C. 2018 ‘Current treatment options for postmenopausal vaginal atrophy’, International Journal of Women’s Health. Volume 10, 387-395.
3. Khanjani, S. Panay, P. 2018 ‘Vaginal estrogen deficiency’, The Obstetrician & Gynaecologist. Volume 21, Issue 1, 37-42
4. Mac Bride, MB. et. al. 2010 ‘Vulvovaginal Atrophy’, Mayo Clinic Proceedings. Volume 85, Issue 1, 87-94