Vulvar and vaginal atrophy has been described as a silent epidemic affecting a large proportion of postmenopausal women who are suffering in silence from this condition.
The disparity between the high prevalence and infrequent clinical diagnosis of VVA is documented in medical practice despite the considerable negative impact on quality of life. This divergence is thought to be primarily a consequence of patients’ unwillingness and/or embarrassment to report symptoms to their healthcare professional and also, from a standpoint of the HCP, the difficulty of approaching this sensitive topic during routine consultations.
Associated with this under-diagnosis is a chronic and progressive condition that may not be addressed for a considerable period of time and, therefore, more likely to undergo disease progression when left untreated.1
In a European study (REVIVE study) a cohort of 3,768 postmenopausal women with VVA symptoms were recruited from four European countries (1000 from Germany, 1000 from Italy, 1000 from the UK, and 768 from Spain).
The inclusion criteria were menopausal (either natural or surgically induced) women, resident in one of the four study countries, aged between 45 and 75 years old, and who had experienced at least one of the vulvar and vaginal atrophy symptoms (dryness, pain with sex, irritation, tenderness, pain with exercise and/or bleeding).1
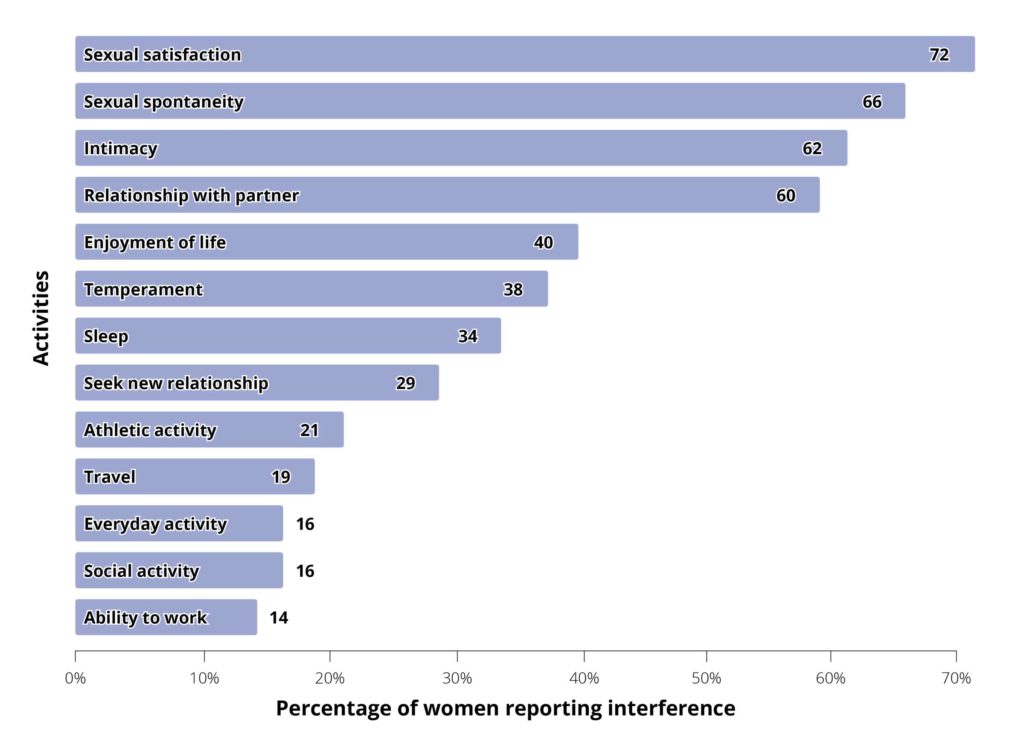
Overall, participants reported that VVA symptoms had the most impact on participants’ sexual satisfaction (72.0% somewhat or very interfering), followed by interferences in sexual spontaneity (66.4%), intimacy (61.9%), and relationship with their partner (59.6%).
– see Figure 2.1
Figure 2. Interference of symptoms of VVA with sexual life and other activities 1
About 60% of the participants stated that symptoms were the same or worse now than when they first appeared, especially with regard to pain during intercourse (76.7%).
All VVA symptoms were rated as quite bothersome, but pain and bleeding associated with sex rated as the most bothersome symptoms.1
Participants also reported that VVA symptoms
made them feel uncomfortable (47.7%), ’old’ (39.9%), frustrated (17.6%) and/or unattractive (14.4%). When asked, “What is the most concerning facet as a result of VVA symptoms?” most participants felt losing their sexual intimacy (40.3%) and their youth (19.1%) were the most significant points of concern.1
Although the majority of participants in the survey experienced one unique symptom associated with VVA, a very high proportion of patients experienced two or more symptoms before consultation with a healthcare professional (HCP). This pattern is related to another observation concerning the waiting time before discussing their problems: between 36% and 50% of participants
(depending on the observed symptoms) waited
more than 6 months to discuss them with
their HCP. This confirms that VVA is an under recognised, under-diagnosed and under treated condition among postmenopausal participants who, although experiencing bothersome symptomatology, quite often do not seek medical help. Vaginal dryness ranked first in the top symptoms to appear in postmenopause, being also the symptom which most participants
clearly identified as being directly related to the
menopause process.1
The discussion of symptoms with HCPs seems the most critical factor for diagnosis and treatment of VVA but there is an inadequacy of fluent communication related to VVA symptoms between patients and healthcare professionals (HCPs) – only 10% of HCPs initiate a discussion on VVA symptoms.1
References
1. Nappi, R.E. et. al. 2016 ‘Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE Survey’, Climacteric. Volume 19, No.2, 188-197