Colecalciferol vs Calcifediol
Figure 1. The molecular differences between calcifediol and colecalciferol.
This molecular alteration underscores significant advantages compared to colecalciferol, as outlined below.
1. Domnisol®(calcifediol monohydrate) offers superior intestinal absorption versus colecalciferol. The intestinal absorption of colecalciferol depends on the presence of bile acids.3 In patients with fat malabsorptive states, the intestinal absorption of colecalciferol may be compromised, whereas Domnisol is absorbed and transported directly into the boodstream via the portal vein. Thus, the absorption of calcifediol is largely preserved3 and is not affected in patients with fat malabsorption deficiencies.4
Domnisol is one step closer in the vitamin D metabolic pathway.
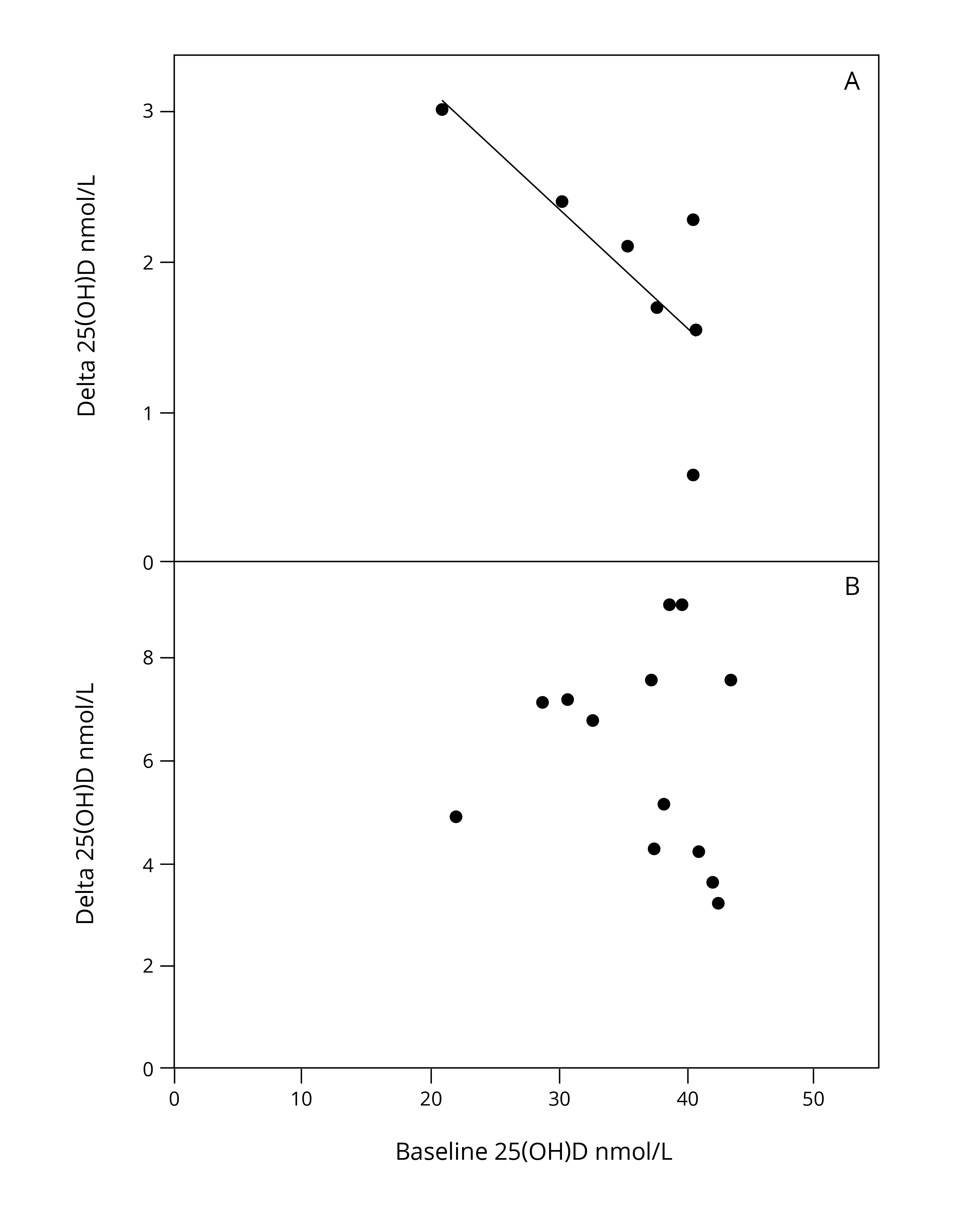
Figure 3. Calcifediol and colecalciferol dose response curves. Mean changes ("delta") in serum 25(OH)D concentration after oral treatment with colecalciferol (A) or with calcifediol (B) according to baseline serum 25(OH)D concentration, as reported in RCTs comparing both oral treatment options.6
6. Domnisol’s pharmacokinetic properties underpin a different frequency of administration in routine maintenance therapy of 1 capsule/month.6
1. Manuel Sosa Henriquez, et al. 2020.Colecalciferol or calcifediol in the management of vitamin D deficiency. Nutrients,12 1617
2. Heike Annette Bischoff-Ferrari, et al.2012. Oral Supplementation with 25(OH)D3 versus vitamin D3: Effects on 25(OH)D levels, lower extremity function, blood pressure and markers of innate immunity. Journal of Bone and Mineral research. Vol. 27, No 1, 160-169
3. Esteban Jodar, et al.2023. Calcifediol: a review of its pharmacological characteristics and clinical use in correcting vitamin D deficiency. European Journal of Nutrition.
4. J.M. Quesada-Gomez, R. Bouillon. 2018. Is Calcifediol better than cholecalciferol for vitamin D supplementation? Osteoporosis International 29, 1697-1711
5. Cianferotti Luisella, et al. 2015. The clinical use of vitamin D metabolites and their potential developments: a position statement from the European society for clinical and economic aspects of osteoporosis and osteoarthritis and the international osteoporosis foundation. Endocrine. 50 (1) 12-26
6. Domnisol SmPC
7. Conti F et al.2012. Adherence to calcium and vitamin D supplementations: results from the ADVICE survey. Clin Cases Miner Bone Metab.;9(3):157–160.
8. Segal E et al.2009. Low patient compliance- A major negative factor in achieving vitamin D adequacy in elderly hip fracture patients supplemented with 800IU of vitamin D3 daily. Arch Gerontol Geriatr.;49(3):364–367.
9. Jackson RD, et al.2006. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med.;354(7):669–683.
10. Rothen JP et al.2020. Oral intermittent vitamin D substitution: influence of pharmaceutical form and dosage frequency on medication adherence: a randomized clinical trial. BMC Pharmacol Toxicol.;21(1):51.
11. Pérez-Castrillón JL, Dueñas-Laita A, Gómez-Alonso C, et al. Long-Term Treatment and Effect of Discontinuation of Calcifediol in Postmenopausal Women with Vitamin D Deficiency: A Randomized Trial. J Bone Miner Res. 2023;38(4):471-479.