ADHD affects an estimated 3.6% of children and 2% of adults in the UK.
The chronicity of the disorder, and impact on function from childhood through to adulthood, is an important aspect of impairment with cumulative effects on self-esteem, mental wellbeing, and health-related quality of life.1 Clinicians who follow individual patients, and their families should be knowledgeable about how ADHD presents, how it causes functional impairment across the lifespan, and ultimately how it can be managed.2
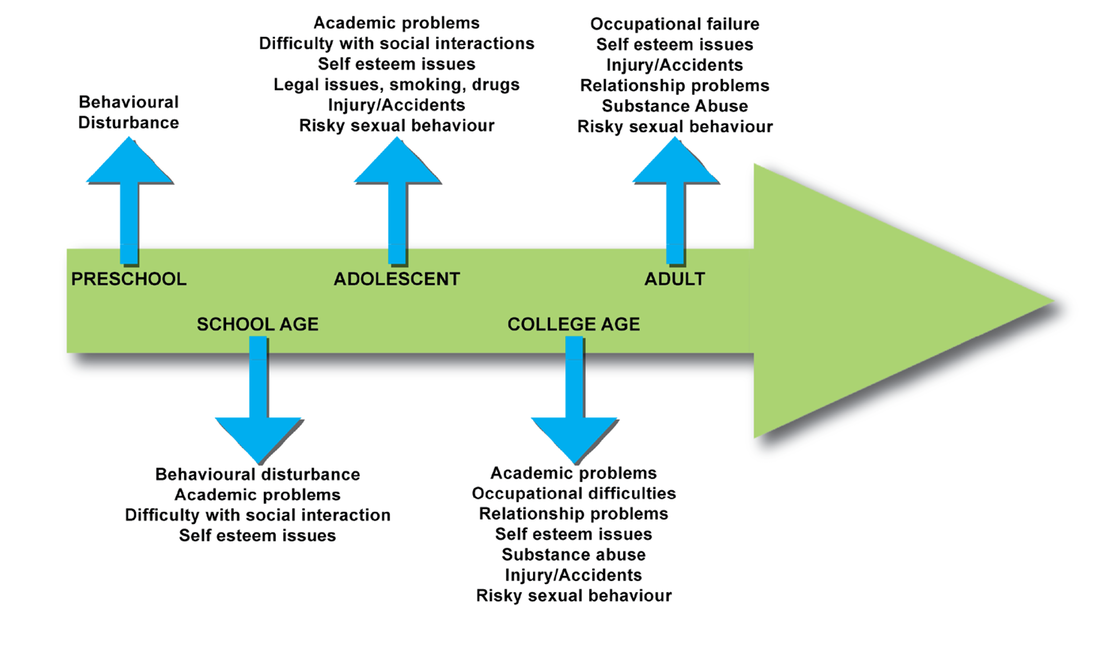
The primary school child with ADHD frequently begins to be seen as being different as classmates start to develop the skills and maturity that enable them to learn successfully in school. Although a sensitive teacher may be able to adapt the classroom to allow an able child with ADHD to succeed, more frequently the child experiences academic failure, rejection by peers, and low self-esteem.3
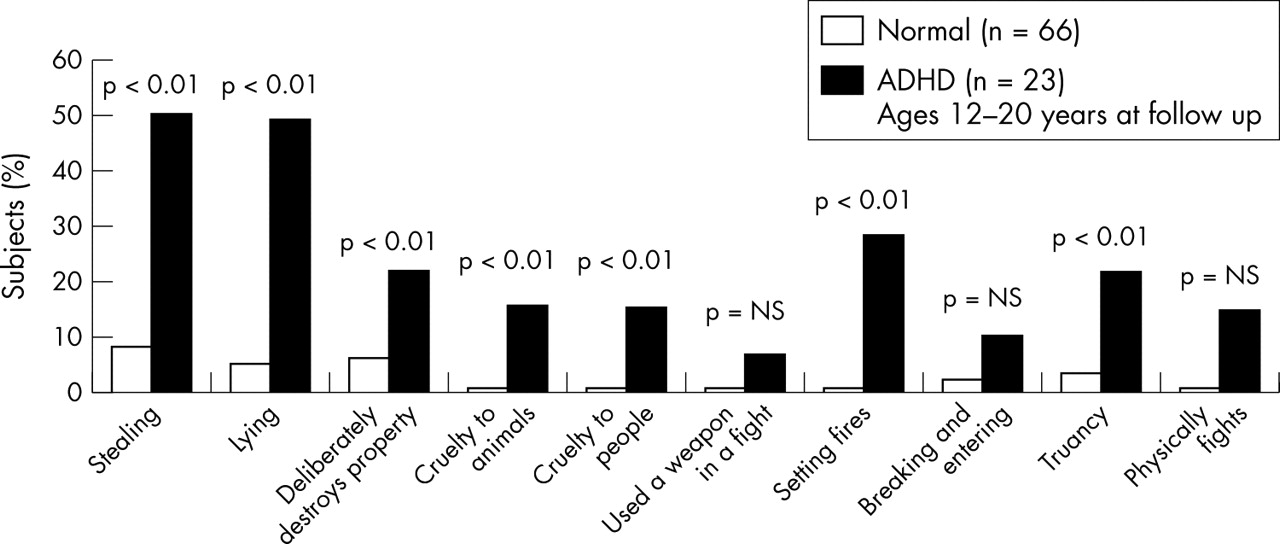
Adolescence may bring about a reduction in the overactivity that is often so striking in younger children with ADHD, but inattention, impulsiveness, and inner restlessness remain major difficulties. A distorted sense of self and a disruption of the normal development of self has been reported by adolescents with ADHD. Furthermore, excessively aggressive, and antisocial behaviour may develop, adding further problems.3
Adults who reported having received a diagnosis of ADHD were significantly less satisfied with their family, social and professional lives.4

Compared with non-sufferers, adults with ADHD are:
Less likely to GRADUATE from university
2x more likely to be ARRESTED
2x more likely to be DIVORCED
More likely to be UNEMPLOYED4
References:
1. UK Adult ADHD Network. Handbook for Attention Deficit Hyperactivity Disorder in Adults. 2013. Springer Healthcare Communications.
2. CADDRA – Canadian ADHD Practice Guidelines, 4th Edition. Canadian ADHD Resource Alliance (CADDRA), 2018
3. Harpin, VA., The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child 2005;90(SupplI):i2–i7.
4. Biederman, J. et al. Functional impairments in adults with self-reports of diagnosed ADHD: A controlled study of 1001 adults in the community. J Clin Psychiatry. 2006 Apr;67(4):524-40.doi: 10.4088/jcp.v67n0403